 Keita Whitten
Keita Whitten KW: When I first branched off into private practice I worked with all clients and diagnoses and accepted all types of insurance. I mean it’s logical, right? I needed to establish myself as a new “clinician.” I had to grow a client base. Still, in the back if my mind, I knew I wanted to do things differently, but I wasn’t sure what that would look like. I simply decided to trust myself and feel my way through the uncertainties. See, the very idea of allowing myself to “feel” my way through clashed with the dominant paradigmatic paradigm. Subsequently, I cannot talk about my current practice decisions or style without first explaining how SE has been a significant part of the process that has guided my current decision.
I remember my Year One of training with SETI (Somatic Experiencing Trauma Institute). I was so excited. It was our first module and the instructor warned us this work would not only change our perspectives about how to work with trauma; it would change us. I had no idea what that meant, but I can remember thinking I was game.
In Year One we were taught basic somatic language--how to observe, to notice what is not being said through somatic cueing. We were taught to treat these cues as places of inquiry and curiosity. This style of observation was familiar. It is a huge component of how Kripalu trains yoga instructors. In both practices, the key was always curiosity instead of causation, learning how to follow sensations, allowing meaning to unfold organically.

I remember breathing a sigh of relief when SE taught that us that environments--like people--are constantly in a dynamic flux between each other, and, in fact, influence each other--including the lens by which we evaluate things. I had already explored this premise as a graduate student in response to being told "qualitative research is nothing more than field research whose conclusions are tainted and biased based on environmental interferences!" And, I was warned I had to guard against "going native.” Well you know me... "going Native?" What the hell? As protest, I just had to take the hard road, again. I had to construct my thesis using methodologies like deconstructing methodologies, participatory action research, and portraiture, in order to demonstrate the fact that not only are environments significant, but they are the lens through which the researcher is conducting the study and they have significant implications on the findings, explanation, presentation, and the use and control of the data.
I know I am veering off subject, but I think is an important divergence. I would go a step further to say, transference and countertransference are how we understand how things work or don’t work. We, people, animals, are constantly evaluating and adapting to the world around us. SE taught us how we do this through our nervous systems each day, each moment. You can’t shut it off. And when we try to, we are missing vital sensory information. For example, we all talk about cognitive dissonance, right? There are lots of explanations about what it is and why it happens, right? Let’s’ agree for a moment with the basic understanding-- it’s a mental discomfort resulting from a clash of values or beliefs. Here’s the thing: What if I said there is also sensory dissonance? No, scratch that. I propose cognitive dissonance is actually a result of sensory discomfort--a stress response to a threat in the external environment. And it shows up as cognitive dissonance when we have overridden our sensory information.
When I have worked with clients who experience explosive anger, I now call it "sensory dissonance." What that means is that they are receiving cues both internally and externally, but trying to override this with reason. Ultimately, whatever they are trying to override with reason--fear, despair or the feelings of betrayal-- will manifest as sideways behaviors and cognitive dissonance. Working through an SE lens, I help people to identify sensory cues both inside and outside of themselves--cues that are often become overridden and lead up to these sideways expressions such as explosive anger and rage. Here's another way to look at this: By the time one is raging, it’s usually because the person has already overridden the sensory inputs--including the role of transferences and countertransferences. Today, somatic psychology is a lens through which I observe everything, everyone--including myself.
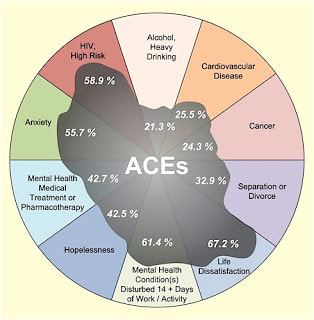
Dr. Nadine Burke, now the first appointed Surgeon General for the state of California, educates about the vital health implications of toxic stress and the wear-and-tear on the immune system, when we do not address trauma and ACEs from a biological, embodied approach.
This data made me pause and think for a moment. I then started to realize that the way we diagnose people is all wrong--the DSM5 is wrong! And, we (therapist, counselors, psychiatrists, all of us) are continuing to prescribe pills, diagnoses and apply psychology like all Western allopathic medicine--WE TREAT SYMPTOMS, not root causes.
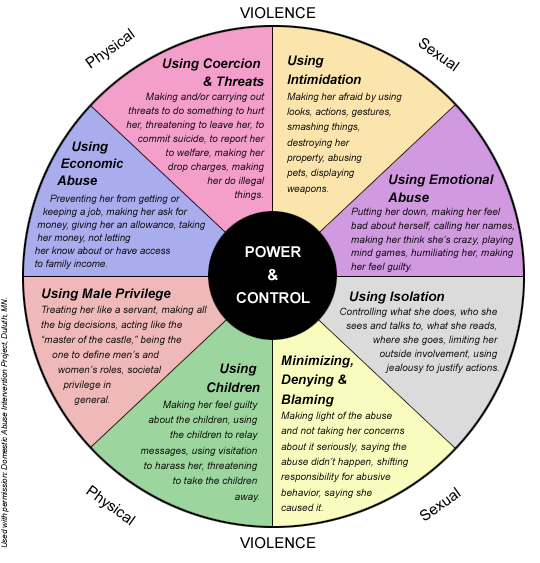
For example, one of my clients taught me a different way to understand bipolor disorder. Assessment took months to uncover contributing external factors like the fact she was exposed to longterm neglect before the age of seven, manipulation like gaslighting, and rape and other sexual abuse--and therefore the needed treatment was not pharmaceutical (in some cases medication may be required initially to calm/stabilize a “wacked” nervous system), but required a holistic approach based an understanding of ACEs and mind-body-soul synergy to support the creation of balance/homeostats. Over time this client began to discover the need for changes in her lifestylem including proper rest, diet changes, and letting go of toxic relationships. With these changes, our sessions, and additional support from homeopathy, she was able to lower her lithium dosage, and her symptoms--including manic flares--began to minimize, which were possible due to her new understanding of the "pain body." The difference was this: These behaviors were there, but less intense, so that she was able to build the capacity to recognize the buildup before the flare-up, allowing the pain body to chillaxe and begin to heal its soul wounds.

You asked about my new THRIVE initiative for 2019. Based on this new understanding, I knew then I could not see all clients because I no longer wanted to do "bandaid work." I wanted to help heal soul wounds. I instantly became aware I had to change how I practiced, including who I saw. And this why today I only work with trauma. Back to the original ACEs population study: With all the recent research about health disparities for communities of color, including women, I realized I wanted to serve the most vulnerable populations--that is, girls and women of color.

CW: I am seeing more and more healers who are not taking insurance. Can you talk about that?
KW: Why don't I take insurance? The simple answer is, SE a, like acupuncture, reiki or homeopathy does not provide enough “empirical” evidence to support how it works for insurance companies to pay for our services. Insurance companies need justification to pay for services. With this justification comes the demand for qualitative, evidence-based practices using levers of variables to determine outcomes. Clinicians have to provide a diagnosis during your first visit, then write up goals and objectives that support the diagnoses, and the come up with arbitrary phrases like, "Client/subject will manage emotional outburst by 50%, by learning how to express their feelings."
We clinicians spend numerous hours trying to add it all up to justify services, and many make it up, and we all know it's BS--but it’s the only way one can get paid. There are insurance discrepancies in terms of what gets paid out, based on what is called "pay-out tiers," which are different with every company. For example, one company might pay you $99 while another might pay you only $65--for the exact same service. And confidentiality? There is no confidentiality with insurance companies. Your information belongs to them to use to qualify or disqualify you.
When I was taking insurance, I received a notice stating I was over-using a diagnostic code based on the demographics of my colleagues who practiced in the area! Can you guess what it was? The code for trauma. This was a real eye-opener! Apparently my colleagues in the field really do not have an informed lens on ACEs and trauma. To be fair, it's probably more of a billing issue, but this means I can't record what I see and suspect, because I will not be paid, and I will not be paid for using a model like SE, because it’s not sanctioned by Big Pharma and the medical communities.
When I feel doubt about what I do, I like to recalled the words of one of my clinical supervisors, “You may not have chosen to work with trauma, but trauma has defiantly called you!" Looking back on my life, I would agree. Each experience has been very informative. And because of my story, I feel I am able to relate to people’s pain, which disarms the power imbalance very quickly.
Nadine Burke says that when people ask her how she can you work with trauma, she gets excited and replies, “because its fundamental hopeful work.” I would agree, and this is especially so working with women of color. I’d like to end with a reference to the works of Anne Wilson Schaef’s book, Meditations For Women Who Do Too Much. Her daily affirmations are a reminder of the vitality of why I do what I do. I know intergenerational healing will take two generations. I will not live to see it, but through the work I do I have hope my grandchildren and great-grandchildren will experience healing through collective and conscious community parenting. I am still unpacking fifty-three years of experiences,
Ashe
Redefining Therapy website











 RSS Feed
RSS Feed
